A 71-Year-Old Man with Throat Pain and Swallowing Difficulty, Atypical Features of Giant Cell Arteritis With Large-vessel Involvement
From Grand Rounds from HSS: Management of Complex Cases | Volume 14, Issue 4
Case Report
A 71-year-old man was hospitalized after 4 weeks of fever, cough, headache, weight loss, and dysphagia. On admission he described severe throat pain and swallowing difficulty, a 15-lb weight loss, daily fever, a mild non-productive cough, and a moderate headache over the top of his head without photophobia, phonophobia, or neck stiffness. He denied temporal pain, jaw claudication, vision changes, or shoulder or hip girdle stiffness. During his 3-week long hospitalization he developed pain in the left anterior neck.
His history included hypertension, hyperlipidemia, and stroke in 2019. He reported no significant occupational exposures, drug use, alcohol use, recent travel, or family history of autoimmune disease.
On presentation, his temperature was 38.4°C; other vital signs were normal. Examination revealed no scalp or temporal artery tenderness, a normal-appearing oropharynx, and tenderness along the left anterior cervical region without lymphadenopathy. His joints were normal. Laboratory studies revealed elevated white blood cell count of 14.9 × 109/L (88% neutrophils), normal hemoglobin level, and elevated platelet level of 511 × 109/L. Autoantibodies for lupus including antinuclear antibodies were negative. Anti-neutrophil cytoplasmic antibodies were negative. Ferritin was elevated to 2941 ng/mL, erythrocyte sedimentation rate was above 130 mm/hr, and C-reactive protein was 29 mg/dL. A broad infectious workup was negative for viral, bacterial, fungal, tick-borne, and parasitic sources of infection. Transthoracic and transesophageal echocardiography ruled out endocarditis and showed no valvular vegetations. Serum protein electrophoresis was unrevealing. Computed tomographic (CT) scanning of the chest, abdomen, and pelvis showed atherosclerosis of the aorta, with a 3-cm infrarenal aortic aneurysm.
Magnetic resonance angiography (MRA) of the head and neck showed soft-tissue thickening of the distal left common carotid artery and left carotid bifurcation (Figure 1). A positron emission tomography (PET)-CT scan identified asymmetric moderate activity of the tracer fluorodeoxyglucose (FDG) along the medial aspect of the left common carotid artery (Figure 2). Skipped areas of mild uptake were also noted along the thoracic aorta wall.
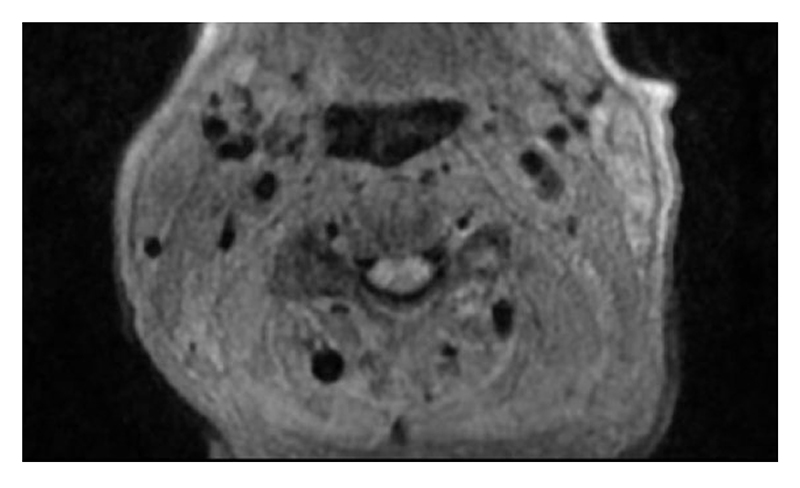
Figure 1: MRA of the neck shows soft-tissue thickening and enhancement surrounding the distal left common carotid artery and left carotid bifurcation without stenosis.
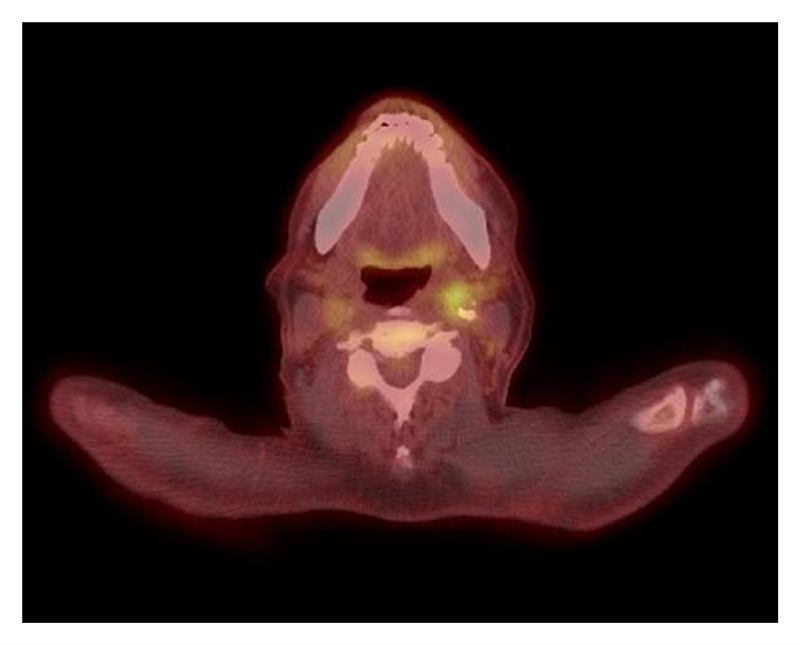
Figure 2: PET-CT scan shows asymmetric hypermetabolic activity along the left common carotid artery.
The patient was diagnosed with giant cell arteritis (GCA) with large-vessel involvement. He received methylprednisolone 1,000 mg IV for 3 days, followed by a prednisone taper. After initiation of steroids, his throat pain, fevers, cough, swallowing difficulty, and headaches lessened. Inflammatory markers normalized. He was started on tocilizumab 6 mg/kg infusion every 4 weeks, and steroids were tapered over 6 months. A repeat PET-CT scan 12 months after treatment began showed resolution of FDG avid areas of the vasculature and a stable aortic aneurysm. He remained on tocilizumab monotherapy without recurrence of symptoms 18 months after initial diagnosis, with a plan that it would be tapered over the next 12 months, with careful monitoring for recurrence of symptoms.
Discussion
GCA is a large and medium-vessel vasculitis often affecting the cranial branches of the carotid artery. Classic presenting symptoms include temporal headache, jaw claudication, visual disturbance, and fever [1, 2]. GCA is the most common form of systemic vasculitis with an estimated lifetime incidence of 0.5% in men and 1% in women [2]. Throat pain and difficulty swallowing, however, are not typical features. A similar presentation of GCA has been described in several case reports [3-7] and a case series [8]. It is hypothesized that throat symptoms in GCA arise from vasculitic involvement of the ascending pharyngeal artery [3, 4]. In our patient, the common carotid artery was inflamed at the level of its bifurcation into the internal and external carotid arteries. Because of the proximity of the carotid bifurcation with the ascending pharyngeal artery, it is likely that throat pain and swallowing difficulty originated from vessel involvement in this area.
This case highlights the importance of considering a diagnosis of GCA in an adult patient with fever of unknown origin and unexplained throat symptoms, even in the absence of classic cranial GCA symptoms.
References
- Grazioli-Gauthier L, Marcoli N, Vanini G, Bernasconi E, Degabriel D. Giant Cell Arteritis among Fevers of Unknown Origin (FUO): An Atypical Presentation. Eur J Case Rep Intern Med. 2021 Feb 9;8(3):002254. doi: 10.12890/2021_002254.
- Chacko JG, Chacko JA, Salter MW. Review of Giant cell arteritis. Saudi J Ophthalmol. 2015;29(1):48-52. doi: 10.1016/j.sjopt.2014.10.001.
- Ling JD, Hashemi N, Lee AG. Throat pain as a presenting symptom of giant cell arteritis. J Neuroophthalmol. 2012;32(4):384. doi: 10.1097/WNO.0b013e318270ffaf.
- Pfeiffer J, Ridder GJ. An old woman with a severe sore throat. J Am Geriatr Soc. 2009;57(6):1118-9. doi: 10.1111/j.1532-5415.2009.02280.x.
- Lemos J, Vaz A, Mos M, Ribeira P, Monteiro A, Henriques P. Temporal arteritis: A confounding diagnosis. Acta Med Port. 2011;24(2):355-360. doi:10.20344/amp.1610.
- Turner K, Wideroff J, Brickman L. Giant cell arteritis characterized by sore throat. BMJ Case Rep. 2021;14(11):e246575. doi: 10.1136/bcr-2021-246575.
- Payen C, Kucharczak F, Favier V. Giant cell arteritis presenting with progressive dysphagia and tongue necrosis. CMAJ. 2022;194(11):E420. doi: 10.1503/cmaj.211483.
- Larson TS, Hall S, Hepper NG, Hunder GG. Respiratory tract symptoms as a clue to giant cell arteritis. Ann Intern Med. 1984;101(5):594-7. doi: 10.7326/0003-4819-101-5-594.

