Glomerulonephritis and Anti-PR3-Antibody Positivity Secondary to Bartonella Endocarditis in a 54-Year-Old Man
From Grand Rounds from HSS: Management of Complex Cases | Volume 14, Issue 3
Case Report
A 54-year-old man with history of seizure disorder, rheumatic heart disease status post bioprosthetic mitral and aortic valve replacements, remote history of parainfluenza endocarditis, and recent diagnosis of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis presented to the hospital with fever and hypotension noted at an outpatient visit. Fevers, fatigue, and night sweats began insidiously 8 months prior. About once per month he had paroxysmal episodes of pain, swelling, and redness in his palm or one of his fingers.
Four months prior to admission the patient’s serum creatinine was 2.0 mg/dL compared to a recent baseline of 0.9 mg/dL. A high titer proteinase 3 (PR3) antibody (294 immunoassay) was detected, and renal biopsy demonstrated active and chronic crescentic glomerulonephritis superimposed on immune complex glomerulonephritis (Figure 1). Laboratory studies were notable for positive serum cryoglobulins, rheumatoid factor greater than 450 IU/mL, and polyclonal hypergammaglobulinemia. Pertinent negative values included antinuclear antibody, anti-glomerular basement membrane antibody, viral hepatitis studies, and blood cultures. He had received outpatient methylprednisolone 1000 mg IV daily for 3 doses.
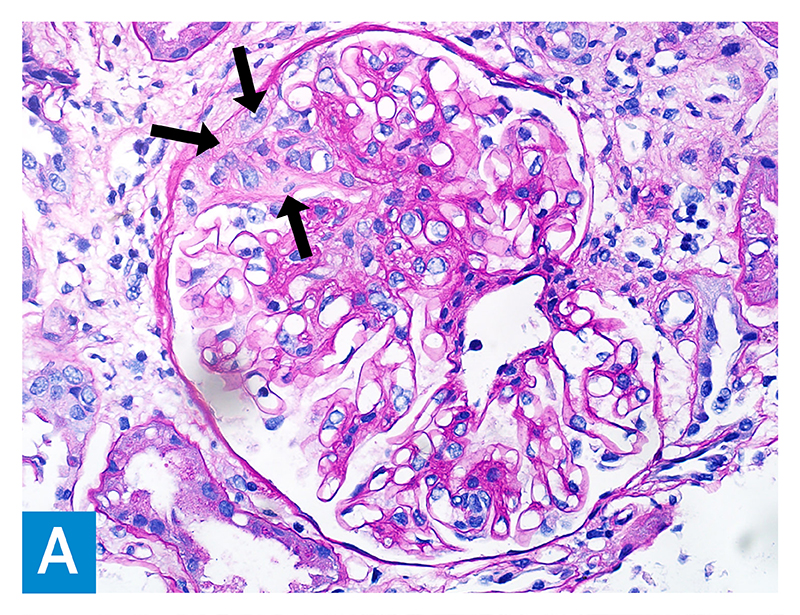
Figure 1A: PAS staining of the glomerulus (400× magnification) showing a fibrocellular crescent in the Bowman space with capsular adhesion (arrows), adjacent to the glomerular capillary tuft, which appears normal in other areas.
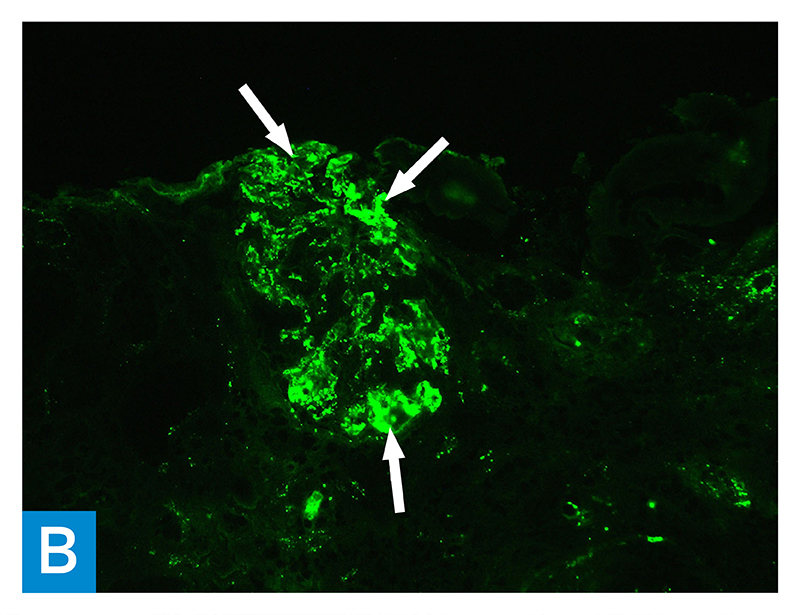
Figure 1B: Immunofluorescence microscopy of the glomerulus (fluorescein-labeled antihuman antibody to C3, 200× magnification) showing granular 3+ C3 staining (arrows) within immune deposits, located in the mesangial areas and focally in the capillary walls.

Figure 1C: Electron microscopy of the glomerulus (12,000× magnification) showing finely granular electron dense deposits within the mesangial areas (circled).
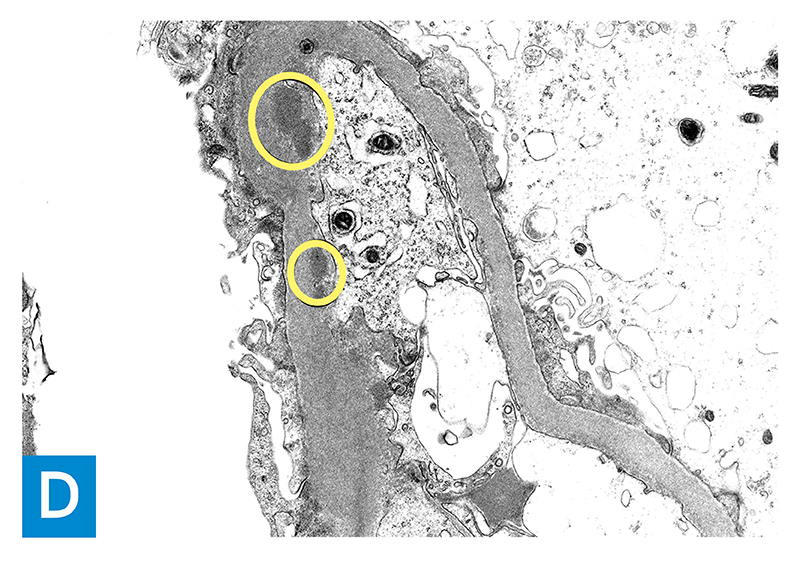
Figure 1D: Electron microscopy (12,000× magnification) showing granular immune complex deposits (circled) in the subendothelial location of a glomerular capillary loop basement membrane.
He denied sinus symptoms, rashes, hemoptysis, numbness, weakness, substance use, or animal exposures. He reported no family history of autoimmune disorders.
Physical examination was notable for enlarged submandibular nodes, poor dentition, a holosystolic murmur heard best at the right upper sternal border, and a hyperpigmented macule on the sole of his left foot. He shared photographs of a previous episode of erythema and swelling at the base of his right fifth finger, 1 cm in diameter.
Laboratory evaluation was notable for normocytic anemia with elevated ferritin of 366 ng/mL, serum creatinine of 3.2 mg/dL, and urinalysis with significant proteinuria, hematuria, and pyuria. C3 levels were low, while C4 levels were normal. Repeat blood cultures were negative. No valvular abnormalities were noted on transthoracic echocardiogram. Transesophageal echocardiogram demonstrated a thin, linear, mobile echodensity on the bioprosthetic aortic valve leaflets; this was suggested to represent either degeneration of the valve or a small vegetation.
Microbial cell-free DNA sequencing demonstrated high levels of Bartonella quintana. This patient was unaware of any lice exposure but did report previously living in a basement he described as not hygienic. He was treated for Bartonella endocarditis with doxycycline and rifampin; constitutional symptoms, renal function, and anemia improved. He subsequently self-discontinued antibiotics for a week, presented with generalized weakness, and was found to have a new mitral vegetation. Antibiotics were resumed and he underwent repeat mitral and aortic valve replacement 4 weeks into antibiotic treatment. After 12 weeks of antibiotic therapy, constitutional symptoms resolved and renal function and anemia improved. He did not demonstrate further manifestations of vasculitis and ANCA serologies normalized with treatment of infective endocarditis; thus, immunosuppressive treatment was not pursued.
Discussion
Given this patient’s history of prosthetic heart valves, a prior episode of endocarditis, 8 months of constitutional symptoms, and possible Osler nodes, there was high clinical suspicion for infective endocarditis, which we posited as an alternative to ANCA vasculitis for explaining crescentic and immune complex glomerulonephritis.
Bartonella-associated immune complex glomerulonephritis is well reported [1–3]. Autoimmune serologies are common in patients with infective endocarditis: in one series of patients, 8% had positive PR3 or myeloperoxidase (MPO), 18% had positive ANCA, and 35% had elevated rheumatoid factor [4].
Typically, infection-related glomerulonephritis is an immune-complex-mediated disease; concurrent ANCA-associated vasculitis has a pauci-immune crescentic pattern. However, in a study of 49 patients with glomerulonephritis due to infective endocarditis, almost half (44%) had pauci-immune immunofluorescence staining, compared with 37% who had endocapillary proliferative glomerulonephritis [5].
In case reports involving infectious endocarditis and glomerulonephritis with positive anti-PR3 antibody, patients generally improved with treatment of the infection without recurrence of vasculitic manifestations [6]. Some have advocated for adding immunosuppression to antimicrobial therapy for severe forms of glomerulonephritis with PR3 antibody secondary to infective endocarditis [7,8]. In this case, the patient was stable and clinically improved with antimicrobial therapy, thus we recommended against immunosuppressive therapy.
References
- Shahzad MA, Aziz KT, Korbet S. Bartonella henselae infective endocarditis: a rare cause of pauci-immune necrotizing glomerulonephritis–a case report. Can J Kidney Health Dis. 2023;10:20543581221150554. doi: 10.1177/20543581221150554.
- Guo S, Pottanat ND, Herrmann JL, Schamberger MS. Bartonella endocarditis and diffuse crescentic proliferative glomerulonephritis with a full-house pattern of immune complex deposition. BMC Nephrol. 2022;23(1):181. doi: 10.1186/s12882-022-02811-w.
- Van Haare Heijmeijer S, Wilmes D, Aydin S, Clerckx C, Labriola L. Necrotizing ANCA-positive glomerulonephritis secondary to culture-negative endocarditis. Case Rep Nephrol. 2015;2015:649763. doi: 10.1155/2015/649763.
- Mahr A, Batteux F, Tubiana S, et al; IMAGE Study Group. Brief report: prevalence of antineutrophil cytoplasmic antibodies in infective endocarditis. Arthritis Rheumatol. 2014;66(6):1672-7. doi: 10.1002/art.38389..
- Boils CL, Nasr SH, Walker PD, Couser WG, Larsen CP. Update on endocarditis-associated glomerulonephritis. Kidney Int. 2015;87(6):1241-1249. doi: 10.1038/ki.2014.424.
- Choi HK, Lamprecht P, Niles JL, Gross WL, Merkel PA. Subacute bacterial endocarditis with positive cytoplasmic antineutrophil cytoplasmic antibodies and anti-proteinase 3 antibodies. Arthritis Rheum. 2000;43(1):226-231. doi: 10.1002/1529-0131(200001)43:1<226::AID-ANR27>3.0.CO;2-Q.
- Sadikoglu B, Bilge I, Kilicaslan I, Gokce MG, Emre S, Ertugrul T. Crescentic glomerulonephritis in a child with infective endocarditis. Pediatr Nephrol. 2006;21(6):867-9. doi: 10.1007/s00467-006-0056-z.
- Sayad R, Elsaeidy AS, Mokresh ME, et al. Immunosuppressant use in infective endocarditis-associated glomerulonephritis: a systematic review. Clin Drug Investig. 2025;45(8):443-529. doi: 10.1007/s40261-025-01461-8.

